Lower back pain or LUMBAGO is one of the most common symptom we see in our day to day practice. Most of the patients don’t take it seriously and end up living a compromised life.
As per the latest study, 75 -85 % of the population experience it at least once in their life. Of those, 50% have a more than one episode within a year.
To understand the pathophysiology, we need to understand the architecture of spine.
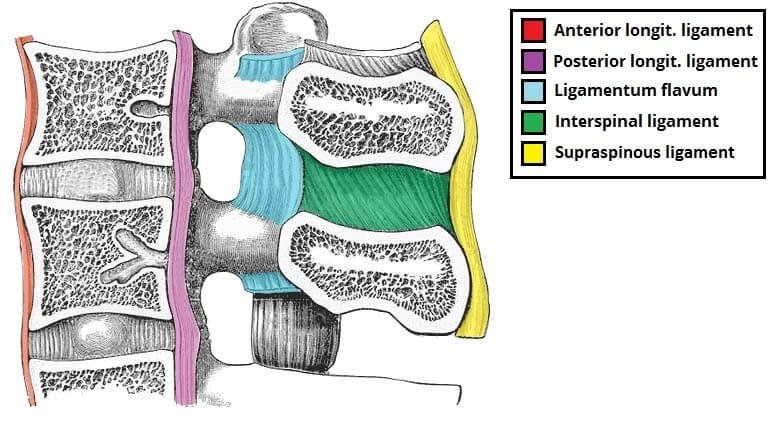
Our spine is a very finely engineered structure, made up of bones, joints, nerves, ligaments, and muscles interconnected to one another and working in harmony to provide a strong support system and flexibility. Any deviation to this complex support system may result into injury and pain.
To treat the pain, it is of utmost importance to treat the cause. So, finding the exact cause will help us in treating the patients with the appropriate treatment option. Lower back pain can further be divided into acute, sub acute and chronic according to the onset and duration.
- Acute pain: Sudden onset and lasts for few days to weeks, and is considered a normal inflammatory response of our body to the tissue damage. As the healing progresses, the pain subsides.
- Sub acute: Lasts from 6 weeks to 3 months. It is mostly a mechanical pain and a proper medical workup is required, if it is bothering the patient in his routine day to day activities.
- Chronic: If pain lasts more than 3 months. A proper work up to know the root cause of pain is a must and accordingly treatment is planned.
Causes:
Muscle or Ligament injury: This is the most common form. It could be an acute sequel due to sudden acute stretch or could be due to repetitive same action like:
- While lifting a heavy object
- Due to fall
- Poor posture over a period of time
- sports injury
Such injuries recover early but not are not causing long-lasting pain, but are quiet severe in intensity.
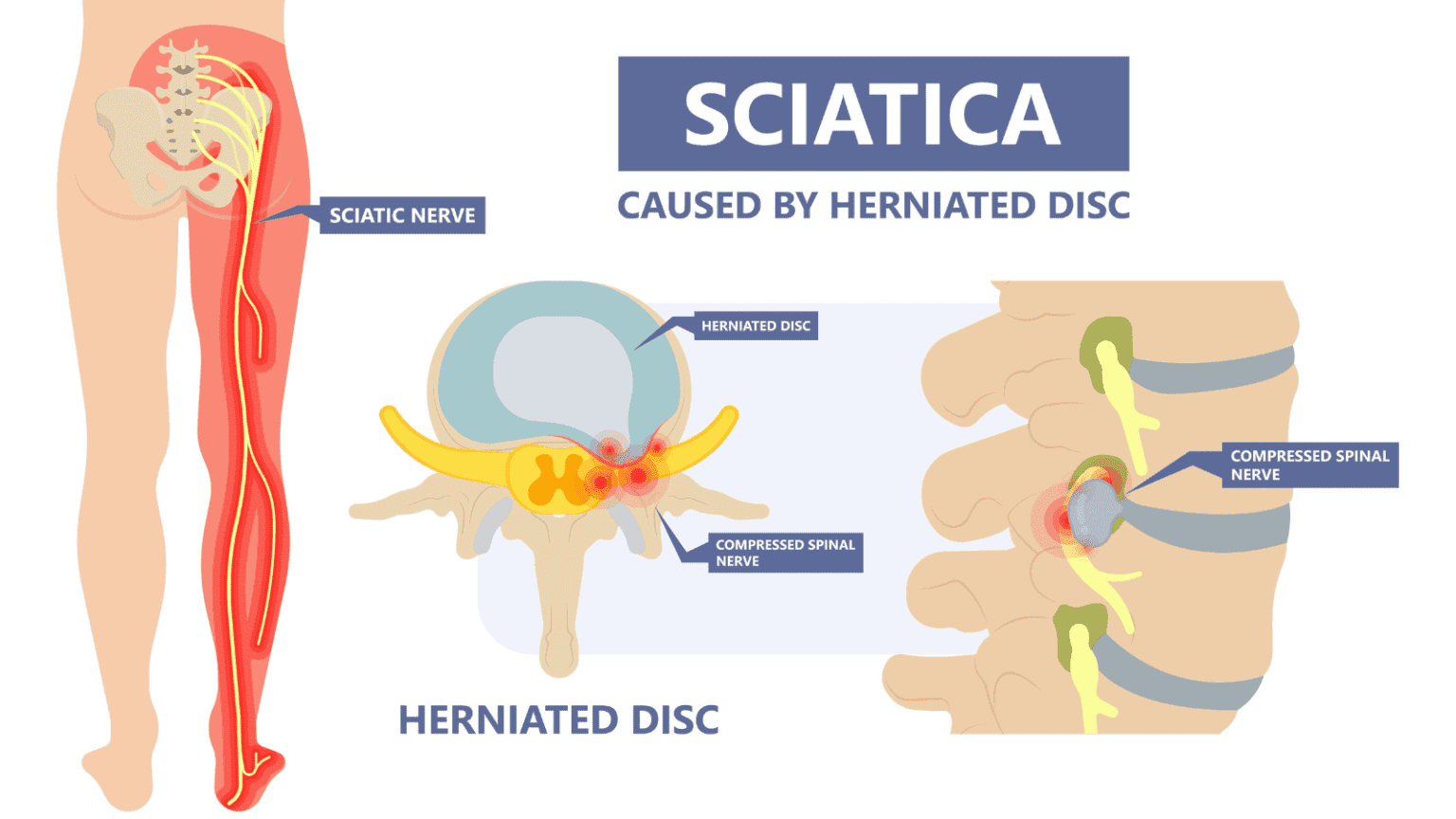
Lumbar Herniated Disc: In between the vertebral bodies of our spine, lies the intervertebral disc. The main purpose of this disc is to act as shock absorbers and provide flexibility to our spine. It is made up the outer though structure called annulus fibrosus and the inner jelly like structure, the nucleus pulposus. Any break in the fibrosus cause the jelly like structure to move out of the defect causing pressure and inflammatory changes on the nerve which results in severe pain.
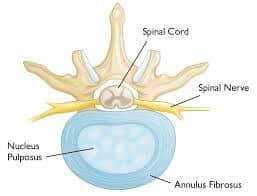
Degenerative disc disease: As our age increases, the disc get dehydrated and loose there elasticity. As a result of which it weakens and results into herniated disc or many times there thickness decreases and collapses leading to lumbar stenosis.

Facetal joint Dysfunction: With age the cartilage along with the capsule in between the facetal joints get eroded and the movements becomes painful as they have a rich nerve supply.

Spinal stenosis: With aging, there is degenerative disc disease which causes thinning of the disc space which causes buckling of the posterior longitudinal ligament, hypertrophy of the ligamentum flavum and development of bony osteophytes. All these causes narrowing of the spinal canal and neural foramina at single and multiple levels, causing spinal canal stenosis.


Spondylolisthesis: In this there is slippage of one vertebral body over another. This again causes narrowing og the spinal canal at the level of slippage. Commonly classified into 5 types i.e. traumatic, iatrogenic, congenital, degenerative, pathologic and isthmic. Most common among them is the traumatic one in which there is fracture of the pars interarticularis (area between the two facets).

Deformity: Kyphosis and scoliosis may lead to back pain if it leads to breakdown of discs, ligaments, facets joints etc.

Traumatic: Acute onset backache secondary to any trauma due to motor vehicular accident or fall from height or sports injury should be thoroughly evaluated.


Osteoporotic Fractures: It usually happens in post-menopausal females. In this there is a cylindrical fracture of the vertebra and is very painful.

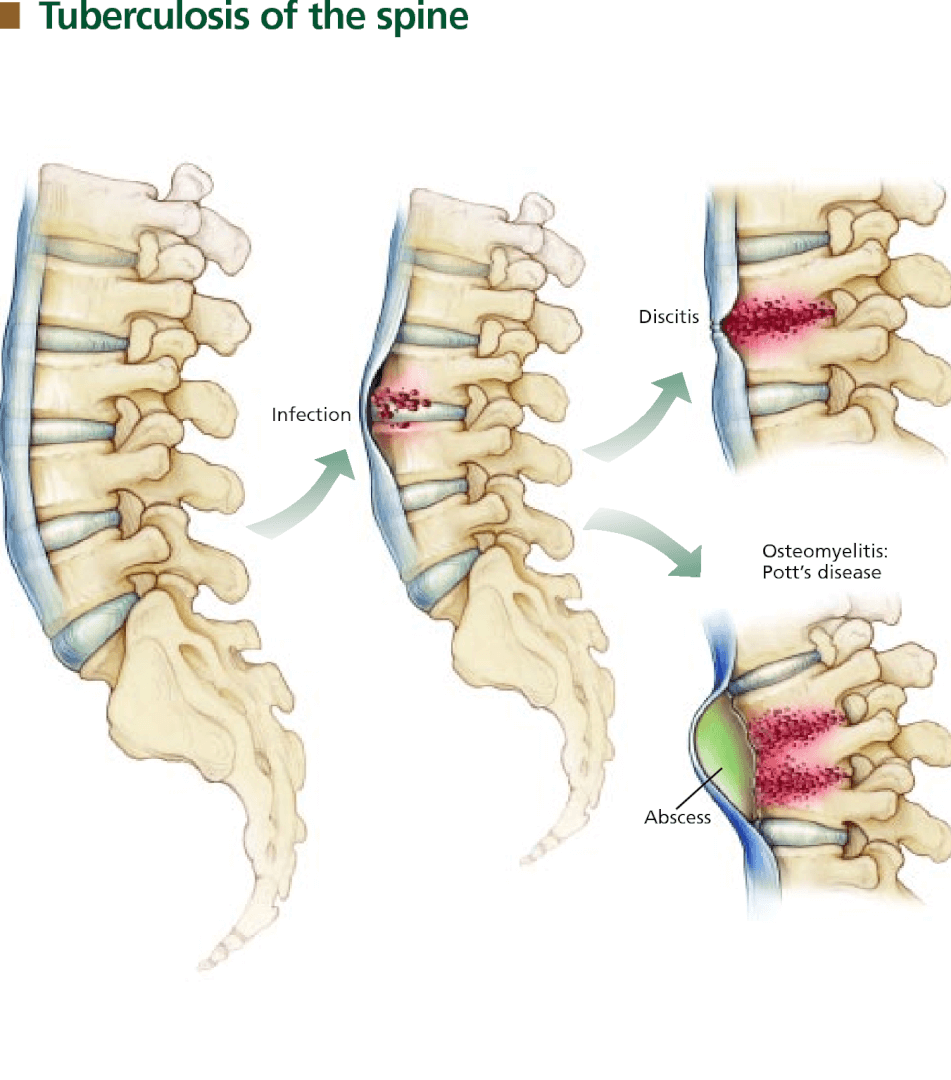
Spinal Infections: Sometimes infections like tuberculosis and pyogenic infections infect the spine and can develop symptoms.
Symptoms:
Backache:
- Dull aching type. It is mainly because of the muscle spasms and restricts the mobility of the person.
- Pain which worsen after prolong sitting. It happens in prolapse intervertebral disc.
- Pain which intensifies on walking for some distance and later the patient has to sit down in a squatting position to relieve the pain. This is neurogenic claudication and is common in canal stenosis. The distance travelled is called the claudication distance.
- Sometimes the patient experiences significant pain after getting up every morning and as the day passes by, the pain is reduced. Occur in facetal orthrosis.
- Pain and discomfort which travel to the buttocks, legs and feet. It is usually on one side of the leg, but sometimes may involve both sides. This is because of the irritation of the sciatic nerve and is called as “SCIATICA”.
If all these symptoms are causing difficulty in the routine daily activities like mobility and sleep, he should consult his doctor soon.
- Symptoms which require immediate medical attention:
- Weakness in lower limbs
- Loss of bladder and bowel control
- Very severe pain following trauma
- Fever with chills and backache
Diagnosis:
History
Once you see your doctor, a thorough history taking is a must. It should include the nature of pain, the aggravating and relieving factors, daily routine activities and lifestyle, job profile, sleeping habits and posture.
General Physical Examination:
A complete physical examination which includes the spinal curvature, range of motion, and few tests like straight leg raising test.
Neurological examination:
Sensory examination in done to check patient’s reaction to light touch, pin prick and temperature over the leg, trunk, buttocks. In motor examination they check the power in flexion and extension of all the joints of lower limbs along with the reflexes.
Radiological Imaging:
X-Ray: Done to see any bony abnormality like fracture, deformity, bony spur or any osteolytic lesion.
Ct Scan: Done in few cases of deformity where they need to calculate the angles of curvature and 3D reconstruction and to get more clearer bony picture.
MRI: It detects any abnormalities in the soft tissues like intervertebral disc, ligaments and muscles. It is always the last investigation to be advised to know the exact pathology and accordingly the management is done.














